Ovarian Cancer Signs: Everything You Need to Know
Ovarian cancer signs are often subtle, which is why the disease has been called a “silent killer.” Symptoms can be vague or easily mistaken for everyday issues like bloating or digestive discomfort. But research shows these symptoms are not truly silent.
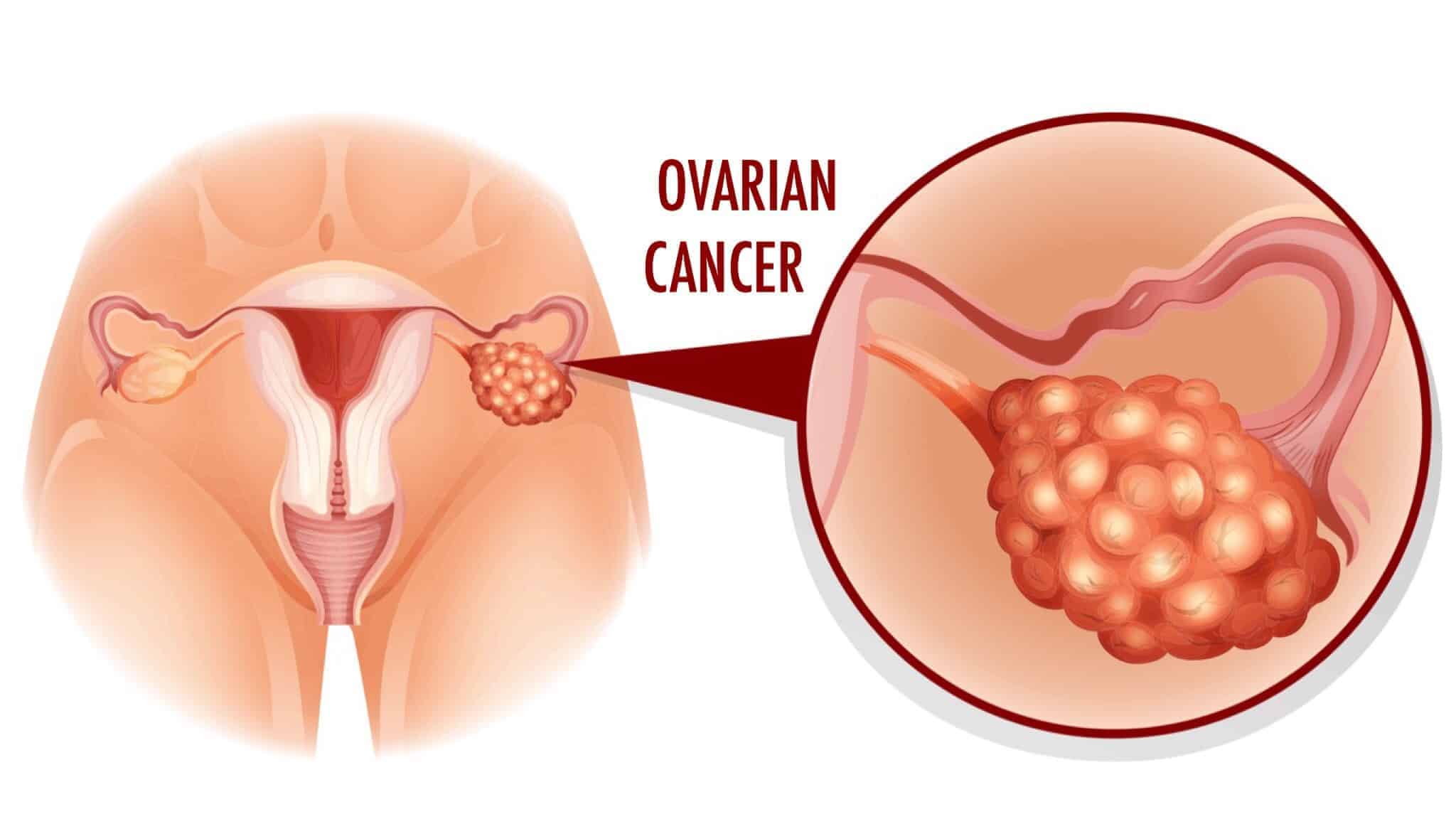
The signs are present—you just need to know what to look for. Ovarian cancer usually begins in the ovaries or fallopian tubes and often isn’t diagnosed until it has already spread. This late detection makes it one of the most serious cancers affecting women, especially after menopause.
However, being informed can make a life-saving difference. In this article, we’ll walk you through the most common signs of ovarian cancer, what causes it, who’s at risk, and how it’s treated. The more you know, the sooner you can act.
Ovarian cancer is not a single disease. It encompasses multiple subtypes, each with distinct cellular origins, behaviors, and treatment responses.
Understanding these types is crucial for accurate diagnosis and targeted care.
“Epithelial ovarian cancer is not a single disease but is composed of a diverse group of tumors that can be classified based on distinctive morphologic and molecular genetic features.”
Dr. Robert J. Kurman, Professor of Gynecology & Pathology, Johns Hopkins University
This type is the most common form, accounting for about 85–90% of ovarian cancer cases. It arises from the surface epithelium of the ovary, fallopian tubes, or peritoneum.
Epithelial tumors are further classified into subtypes:
These constitute about 5% or less of ovarian cancers and arise from the cells that form eggs.
Most often seen in teenagers and young women, germ cell tumors tend to grow quickly but respond well to treatment:
These rare tumors, around 2–5% of cases, originate from the ovarian stroma, which supports hormone-producing cells:
They often produce estrogen or testosterone, leading to symptoms such as abnormal uterine bleeding or virilization. They usually grow slowly and are often diagnosed at early stages.
These cancers, once considered separate diseases, now share biological and clinical similarities with epithelial ovarian carcinoma.
In fact, many high-grade serous cancers once thought to originate in the ovary now appear to begin in the fallopian tubes.
Although once labeled a “silent disease,” ovarian cancer frequently presents with symptoms early on. The challenge lies in their subtlety and overlap with common gastrointestinal or urinary issues.
Recognizing persistent symptoms (nearly daily) and progressive (worsening over time) can lead to earlier diagnosis and better outcomes.
Chronic bloating that lasts for more than a few weeks is one of the most commonly reported early signs of ovarian cancer.
Unlike normal, fluctuating bloating from diet or menstruation, this type tends to worsen over time and doesn’t go away with simple lifestyle changes. Tumor growth or the accumulation of ascitic fluid in the abdominal cavity are frequently the cause.
Pain or a sensation of pressure in the lower abdomen may signal the presence of a growing mass. This discomfort is usually dull and persistent—not sharp or cramping like menstrual pain.
It may also be accompanied by tenderness or a sense of heaviness in the pelvic region, especially as the tumor expands or presses against nearby structures.
Also known as early satiety, this symptom involves feeling full after eating only small amounts of food. It can develop when tumors press against the stomach or intestines, leaving little room for normal digestion.
Such behavior often leads to reduced food intake and unintended weight loss, especially in later stages of the disease.
Ovarian tumors can grow large enough to press on the bladder, mimicking the symptoms of a urinary tract infection.
Women may feel the need to urinate often, sometimes even waking at night to go, or experience a sudden urgency that’s difficult to control. Importantly, the phenomenon occurs without an increase in fluid intake.
Constipation, diarrhea, or alternating between the two can occur as tumors put pressure on the bowels or affect peristalsis.
People often overlook this symptom or mistakenly attribute it to diet changes, IBS, or stress. If persistent, it can indicate growing pressure in the abdominal cavity or peritoneal spread of the cancer.
Ongoing fatigue is more than just feeling tired. Chronic inflammation, cancer-related anemia, or the body’s metabolic response to the tumor can cause ongoing fatigue in the context of ovarian cancer. Women often describe a lack of energy that doesn’t improve with rest, making it difficult to maintain daily routines.
🟤 Pain during intercourse
Dyspareunia, or painful sex, can be a lesser-known symptom of ovarian cancer, particularly when tumors affect the pelvic organs or surrounding tissues.
The pain is often deep and persistent, not just surface-level discomfort. It may also be associated with post-coital bleeding, a concerning sign that should prompt immediate medical evaluation.
Bleeding between periods, excessively heavy periods, or any postmenopausal bleeding should never be ignored.
While more often linked to uterine conditions, these symptoms can occur when ovarian tumors disrupt hormonal balance or invade adjacent reproductive tissues.
Hormone-producing tumors, such as granulosa cell tumors, are particularly known for triggering abnormal bleeding.
A woman might notice her pants fitting tighter due to fluid buildup, even if her overall weight appears stable. Such behavior can mask simultaneous muscle loss or malnutrition.
On the other hand, rapid weight loss—especially if unintended—may indicate cancer-related metabolic changes. When paired with other symptoms, one should take either extreme seriously.
Back pain may develop as the cancer spreads to lymph nodes or the lower spine. It can feel dull and persistent, often worsening with time.
In later stages, blocked lymphatic or venous drainage may cause one or both legs to swell—known as lymphedema—especially if tumors press on major blood vessels.
Ovarian cancer is often diagnosed after symptoms arise, as there’s no standard screening test for the general population. Diagnosis involves a combination of physical exams, imaging, blood markers, and sometimes surgery.
When symptoms are persistent and concerning, doctors use these tools to evaluate and confirm the presence of cancer.
The exact cause of ovarian cancer isn’t always clear, but research has uncovered key contributing factors. Most cases are linked to genetic mutations or cellular damage that accumulates over time.
Some causes are inherited, while others relate to lifelong hormonal exposure or inflammation.
🧬 BRCA1/BRCA2 mutations
🧪 Lynch syndrome
🔁 Incessant ovulation
🌸 Estrogen exposure
🧫 Fallopian tube origin
🔥 Chronic inflammation
🌿 Endometriosis
Ovarian cancer is often diagnosed at a later stage, not because it’s silent, but because its early symptoms can mimic common digestive or urinary issues.
There’s currently no reliable screening test for average-risk women, which means diagnosis usually begins only after symptoms become persistent and concerning.
Doctors typically use a combination of tools to evaluate suspected cases. These include a pelvic exam, transvaginal ultrasound, and a blood test for CA-125, a protein that may be elevated in ovarian cancer.
A biopsy or laparoscopy may be required to confirm the diagnosis and identify the type and stage of the cancer if imaging or lab results raise concerns.
In advanced cases, procedures like paracentesis can analyze fluid buildup (ascites) for cancer cells. The key is early symptom recognition and prompt medical evaluation.
A few key factors raise your risk: age over 50, a family history of ovarian or breast cancer, inherited mutations like BRCA1/BRCA2, endometriosis, never having been pregnant, long-term hormone therapy, obesity, and possibly talc use. Having one or more doesn’t mean you’ll get cancer—but awareness can help with early detection.
Ovarian cancer is staged from I to IV.
Staging helps guide treatment and estimate prognosis.
Treatment depends on the type and stage. Most women undergo surgery to remove tumors, followed by chemotherapy. Advanced cases may also include targeted therapies like PARP inhibitors or clinical trials. Some early-stage cases, especially in younger women, may allow fertility-sparing options.
Survival depends on the cancer type, stage, and overall health.
High-grade serous carcinoma has the lowest survival, while early-detected subtypes fare better.
Yes—some strategies may lower your risk. These include using birth control pills, pregnancy and breastfeeding, removal of fallopian tubes (for high-risk women), and avoiding unnecessary hormone therapy.
Maintaining a healthy weight and managing inflammation may also help, though no method guarantees prevention.
No. Bloating is common and often caused by diet, hormones, or digestion. But if it’s persistent, happens daily, and worsens over time, especially when combined with other symptoms like pelvic pain or appetite loss, it should be evaluated. In these cases, bloating could be an early sign worth investigating.
You don’t have to be unprepared for ovarian cancer. The signs of ovarian cancer are real, the science is advancing, and taking early action can significantly impact outcomes.
While you can’t control every risk factor, you can stay aware of your body and speak up when something feels off.
Let this knowledge empower you—not overwhelm you.
Talk to your doctor. Know your body. Stay informed. 💛
Related Articles